In the final episode of this six-part limited series documentary, about the battle for PrEP access in the UK: What we can learn from the fight for PrEP in future sexual health and queer health provision, from gender-affirming care to DoxyPEP.
The Other Blue Pill has covered a lot of ground on the history of PrEP and where we're at with it now. But what does its future look like?
The hidden history of PrEP shares a lot of lessons on how we can do things differently to ensure all of our sexual health needs are met.
This week, we look at the exciting innovations in sexual health provision that are going to further change and revolutionise the sex lives and healthiness of so many people. We also explore the next battle in HIV and sexual health - DoxyPEP, with guests:
- Deborah Gold - Chief Executive of National Aids Trust
- Will Nutland - Co-founder of PrEPster and Director of The Love Tank
- Dan Ellis - Actor and director, What The Pox? guest
- Benjamin Weil - Head of Research and Community Knowledge Generation at The Love Tank
- Florence Eshalomi - MP for Vauxhall in 2019 general election
Credits: Hosted and written by Phil Samba. Produced by Jamie Wareham. A QueerAF Production for the Love Tank, with support from National Aids Trust.
Resources:
Full show notes, with sources
Phil Samba (Host)
Nearly twenty years after it was first discovered that PrEP could prevent HIV.
Almost a *decade* after these drugs were first prescribed in the US.
And just four months before the end of the PrEP Impact trial.
PrEP *FINALLY* became available on the NHS in England.
Despite a somewhat delayed rollout due to the COVID-19 pandemic by the end of 2022 - 86,324 people were taking PrEP in England according to annual official statistics data from UK Health Security Agency.
That’s 85% of the people the UK Health Security Agency considers as quote “in need” of PrEP.
This was excellent news after a long legal fight, multiple trials, and campaigning from clinicians, researchers, and community activists from grassroots organisations in the HIV and sexual health sector.
But. The majority of people on PrEP in England in 2022 were white, cis, gay men.
In fact, almost 75% were according to more stats from UK Health Security Agency.
And actually, more people than the UK Health Security Agency say would benefit from PrEP.
And as we revealed last time in episode five, while this means many white queer men can get and take PrEP - despite the barriers to accessing it that exist even for them - there are all sorts of people from different communities that are still locked out of the benefits of this life-saving drug.
Throughout this documentary series, we’ve talked about queer men, especially Black queer men, trans and non-binary people, women, especially Black women and trans women. They are all disproportionately affected by HIV.
So are some groups of sex workers, migrants and drug users and they all have different barriers that mean PrEP uptake is lower in these communities for different reasons.
So how can we fix this and ensure anyone and everyone who needs PrEP can access it?
It may feel insurmountable but we have the tools to fix all of this - we just need to use them.
At The Love Tank, our community-based research on the sexual health needs and experiences of young queer men in London found that the barriers to taking PrEP were:
Stigma about PrEP, access difficulties and badly perpetuated myths about PrEP
Meanwhile, another report from the UK Health Security Agency found the impact of STIs remains greatest in young people aged 15 to 24, queer men and Black people.
Since we’re talking about where we are now with PrEP, it made me curious about where we could be, and what could that future look like.
For example, many people take PrEP in a pill form - but what a lot of people do not know is that there are new and emerging ways of taking PrEP.
Will Nutland
So there's lots of research that shows that not everyone wants to take PrEP using an oral pill and that if we can develop different methods of taking PrEP just in the same way as we've done with contraception, then PrEP is likely to be more acceptable and more people are therefore likely to start taking it.
Phil Samba (Host)
Will Nutland, Director of The Love Tank
Will Nutland
So we know, for example, that some people don't want to hold a bottle of pills at home.
They might have a partner that they don't want to share their PrEP use with, or they may live at home with family members, or they may travel regularly and are scared of taking what's in essence seen as an HIV medication across borders with them.
Phil Samba (Host)
There are also new technologies in sexual health coming up.
Will Nutland
And so there are a range of new technologies that have both been approved and are in development. They include a vaginal ring that can be inserted into the vagina and left for a period of around four weeks. The benefit of that is it's discreet, your partner or partners may not even know that you've inserted it. And also if it's already inside you, there's not the issues of forgetting to take the medicine like there might be if you're taking an oral formulation of PrEP.
Phil Samba (Host)
And for people who face barriers to PrEP, and those who aren’t good at remembering to take it, that’s where a new injectable long-acting version of PrEP could become invaluable.
Will Nutland
There's the recent introduction of a two-monthly injection called long-acting injectable PrEP using a formulation of PrEP called Capitegravia. And that's now being rolled out in many parts of the world, in some parts of the USA. It's routinely available. It's not yet available on a routine basis in any parts of Europe.
And that's partly because of cost, but also, the drawback of using long-acting injectable PrEP is that you have to go into a clinical service every two months to have that injection administered to you. Right now you can't self-administer long-acting injectable PrEP in the same way as you might want to with oral PrEP. And that means that an individual who wants to use that formulation of PrEP, if they're taking PrEP all of the time, will have to go for six clinic visits a year. Whereas in someone like London at the moment, someone who's using oral PrEP can generally get away with about one clinic visit a year if you're lucky and then have your PrEP administered or delivered in ways that don't involve going to a sexual health clinic.
Phil Samba (Host)
Actually, in June 2024, pharmaceutical company Gilead announced that no HIV infections were seen in over 2000 young women and adolescent girls in South Africa and Uganda they were given twice-yearly injections of its innovative drug, lenacapavir, as PrEP, in its PURPOSE 1 study. In the near future, someone who wants PrEP would only have to visit a clinic twice a year to get it.
Will Nutland
The other exciting development is looking at formulations of PrEP that could also serve as a contraceptive method and then you kind of get a two-for-one deal there. So by inserting, for example, a vaginal ring that acts as a formulation of HIV prevention, you are also using it as a form of contraception. And that's an exciting development and is likely to be a formulation of PrEP that is particularly attractive to many people.
The current challenges with new formulations of PrEP, however, are that they are generally a lot more expensive. The current challenges with new formulations of PrEP, however, are that they are generally a lot more expensive for either individuals or health services to buy. And then if that particular formulation of PrEP needs a clinic visit around it, there's an additional cost either again to an individual if they're paying for their own health care or if they're going through their health service, there's an additional burden on those health services.
Phil Samba (Host)
But this isn’t the only innovation coming into the sexual health space.
Will Nutland
And just around the horizon, there's increasing research and development work being done on the potential for using a vaccine that is currently used against meningococcal B for gonorrhoea prevention. And again, it's likely that that vaccine will start to be introduced in places like London and the rest of the UK in the coming 12 months.
So there'll be an offer probably in sexual health clinics for groups of people who are most likely to be involved in gonorrhoea exposure to be offered that vaccination through the National Health Service.
All of these tools offer huge potential, but they need to be provided in ways that are accessible, that are equitable. They need to be offered for everybody who needs them and everybody who wants them.
Phil Samba (Host)
These new emerging ways of taking PrEP could revolutionise the opportunities for people to have even more options to take their sexual health into their own hands.
Time and time again, we’ve seen how ready, queer men are to take up new prevention tools and take them seriously.
There was a major global MPOX outbreak in 2022, and though it can affect anyone it primarily affected gay, bisexual, and other men who have sex with men, probably due to dense sexual networks as MPOX can be passed on through skin-to-skin contact.
Formerly known as monkeypox it’s a rare infection that usually occurs in Central and West Africa and like I said is often passed on through skin-to-skin contact, and on rare occasions through sharing bedding and towels.
There was an initial push to get the government to provide vaccines but as soon as they were made available to protect against MPOX, we saw so many gay, bi and queer men in big cities queue up for them.
Dan Ellis
I think we were told from my point that time in the morning, it’d be about a two and half hour wait which seems like a lot but I’ve queued for three hours to get on Nemesis at Alton Towers so it didn’t bother me. I was absolutely fine with that.
The gents in front of me asked “how quick does the queue go down?” And the health worker who was responding to questions said we’re getting through 60 people per hour and his response was so divine, that’s why I’m here. And that kind of set the tone for the day, I think.
That people had planned their outfits - great. I had a jacket with a stain on it which was a bit suspect but I hoping it might help my case if it did come down to if I would get it or not, I was eligible.
And also, quite a lot of handsome people in the queue, not gonna lie. I know you shouldn't when looking for vaccines and stuff like that, you shouldn’t be looking to pull but you also know they put out so double win really for me.
Phil Samba (Host)
This isn’t the first time a QueerAF podcast has mentioned MPOX either - in case you didn’t catch What The Pox? That was a clip from the documentary investigation into the MPOX outbreak.
It painted the bigger picture of a crumbling and underfunded sexual health service in the UK and England. But crucially, it spoke about how we had the tools to prevent sexual health issues like MPOX, and HIV.
Will Nutland
For the last two or more years, seen outbreaks of MPOX or monkeypox in different parts of the world.
Phil Samba (Host)
Will Nutland from The Love Tank.
Will Nutland
And in the UK, there's a hope that MPOX vaccination will, across the next 12 months or so, be introduced as a routine vaccination through sexual health clinics. My concern is that if we don't start to routinely offer MPOX vaccination, our population protection against MPOX will diminish and will diminish again.
And we could end up seeing outbreaks of MPOX, particularly in people who missed those first rounds of vaccinations that we saw over the last two years or so. So people who were not sexually active two years ago who become sexually active and then may become exposed to MPOX. We really need to see that routine vaccination happen.
Phil Samba (Host)
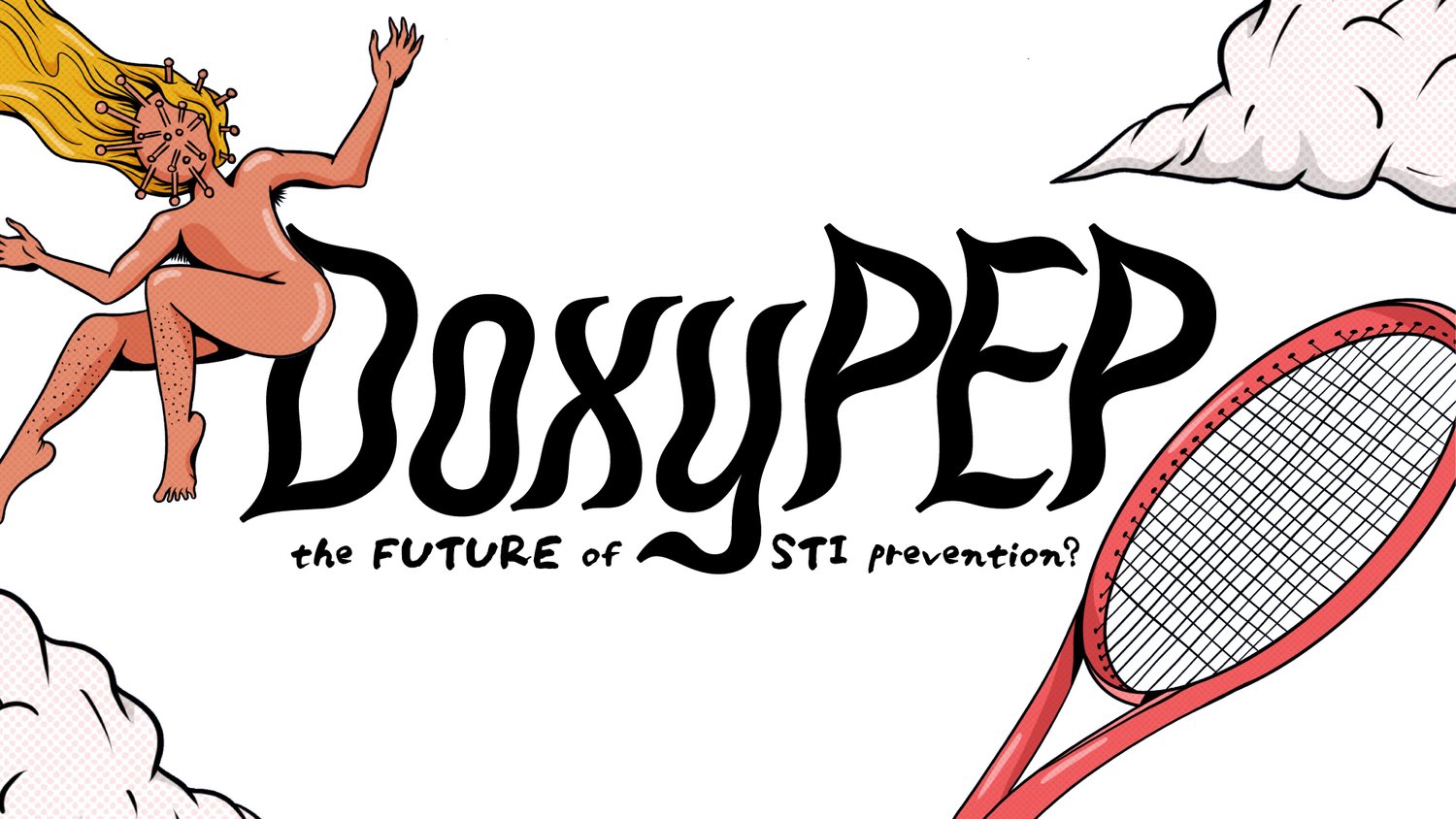
We have the lessons from the fight for HIV treatment, the fight for PrEP, and the fight for MPOX vaccines to inform us about the next emerging sexual health battle - DoxyPEP.
Will Nutland
One of the other exciting developments on the horizon is the potential of something called DoxyPEP or Doxycycline being used as a way of preventing bacterial sexually transmitted infections by somebody taking 200 milligrams of an antibiotic called doxycycline within about 24 hours of potentially being exposed to a bacterial STI.
There are incredibly exciting developments around the potential for DoxyPEP, particularly if it can be targeted in those populations that have the highest incidence of bacterial STIs, including gay and bisexual men in very highly sexualised networks with lots and lots of partner exchange.
And it's exciting because DoxyPEP is being shown to particularly be effective as a prevention against syphilis. And until we have other ways of preventing syphilis, then DoxyPEP offers us a stepping stone, a kind of stopgap until something like a vaccine might be developed.
Ben Weil
Hello, my name is Dr Benjamin Weil. I am the Head of Research and Community Knowledge Generation, here at The Love Tank.
Phil Samba (Host)
That’s my colleague, Ben. They’re an incredible researcher who has done lots of health promotion work on DoxyPEP in an essay, an online guide and a booklet, it’s not currently prescribed in the UK on the NHS but we know some people are already using it or thinking about using it.
Ben Weil
So DoxyPEP isn't licensed for use currently in the UK, although we know lots of people are already using it but it has been approved and licensed for use in part based on the strength of the data that's come from clinical trials, as well as the acceptability within the communities that it's recommended for in Australia and parts of the United States, including Chicago and Seattle.
Phil Samba (Host)
I wanted to understand what we know about DoxyPEP and at the time of this recording in the summer of 2024, there are *three* major clinical trials showing DoxyPEP works.
Ben Weil
There have been at the time of this recording three major clinical trials that show us that DoxyPep works. Two of those clinical trials have taken place in France, one is called Ipergay and the other is called DoxyVac and the other major trial was called DoxyPEP and took place in the United States. And what both of those trials show us is that DoxyPEP is very effective at preventing, in particular, chlamydia and syphilis.
It can prevent upwards of three-quarters of infections of chlamydia and syphilis and also shows good efficacy at preventing gonorrhoea, although slightly less than chlamydia and syphilis, able to prevent around half or just over half of cases of gonorrhoea.
Phil Samba (Host)
This is incredible! But who are the people using it?
Ben Weil
We know for instance from ongoing survey data that, you know, since the mid-2010s onwards, at least 9 to 10% of gay men who use HIV PrEP also report already using some form of antibiotic as an STI prevention tool. So that suggests that you know, DoxyPEP or other forms of prophylaxis, although DoxyPEP is the one that is sanctioned and has evidence to suggest that it works, has been being used for some time.
Phil Samba (Host)
Prophylaxis is treatment given or action taken to prevent disease. An example of this can be PrEP, remember PrEP stands for Pre-Exposure Prophylaxis. Pre as in before, exposure as in exposure to HIV and prophylaxis as in medication that prevents HIV by taking it before and after sex.
Doxy is short for doxycycline, the antibiotic. PEP is short for post-exposure prophylaxis: post means after, exposure means potential exposure to STIs and prophylaxis again means treatment given or action taken to prevent disease.
Ben Weil
The other thing to note is that even in Ipergay, which is that study that I've mentioned where the authors weren't entirely clear about the origins of DoxyPEP and why they were exploring it in the study, even in that study, when the researchers looked at the placebo arm of the trial, so that's the arm of the participants in the trial who were given a pill that wasn't Doxycycline, to use as a form of prophylaxis.
The authors found that a significant percentage, almost, I think 10% of participants in that arm already had doxycycline in their blood. Of course, some of those people could have been using doxycycline as a form of treatment, but it does suggest, once again, that a significant proportion of those individuals in that trial were already possibly using DoxyPEP.
So, taken together, we have some evidence that begins to triangulate on the suggestion that DoxyPrEP may have been invented by queer communities, which is quite exciting and interesting.
Phil Samba (Host)
Now I can almost hear what you’re thinking right now. Let me guess, “this sounds pretty similar to the fight for PrEP” - I’m happy to inform you that you‘re absolutely right, it does.
But before we get to that, there’s also a lot of chat and questions about antibiotics and antimicrobial resistance - and with Doxy PEP, that’s an important distinction to PrEP’s journey.
Ben Weil
There is a possibility that the use of DoxyPEP could increase or accelerate what we call antimicrobial or some people call antibiotic resistance. And that's because DoxyPEP involves the use of an antibiotic, in this case, doxycycline, and what we know about antimicrobial resistance which by the way is a property of bacteria so it means when a bacteria acquires genetic material that means it's capable of resisting or is no longer killed by the antibiotics that normally kill it.
Phil Samba (Host)
And how does antimicrobial resistance even happen?
Ben Weil
And what we know about antimicrobial resistance is that it's accelerated any time that antibiotics are used pretty much but in particular when they're used in ways that are considered to be quote-unquote, unnecessary or not in the manner in which they're prescribed. So what we might term overuse of antibiotics.
Phil Samba (Host)
And where are we overusing antibiotics?
Ben Weil
Probably the most significant and most important example of this would be the use of antibiotics in intensive farming. About two-thirds of all antibiotics worldwide are used on livestock and we know that that drastically accelerates the rate at which bacteria and really, really common bacteria that we need antibiotics to treat, acquire antimicrobial resistance.
Phil Samba (Host)
Doxycycline is also routinely prescribed to teenagers who have acne and those people deserve treatment that works for them. But we don't see widespread conversations and concerns about prescribing doxycycline in relation to teenage acne. Efficacy data actually shows that DoxyPEP is much better at preventing STIs than it is at curing or treating acne.
Ben Weil
So because DoxyPEP involves taking antibiotics, there is always a chance that its use could lead to an uptick in antimicrobial resistance. And I should mention this is particularly important because gonorrhoea, which is one of those bacteria that I've already mentioned that DoxyPEP can prevent, gonorrhoea already shows some signs of resistance to Doxycycline or in fact tetracyclines which are the class of antibiotic that doxycycline belongs to.
So there is that risk and it's something that we all need to be cognisant of and I think work together and I mean we including communities that use DoxyPEP policymakers, community organisations, workers in sexual health all work together to develop you know equitable and fair strategies for monitoring antimicrobial resistance in relation to DoxyPEP.
Phil Samba (Host)
Ben says that when it comes to DoxyPEP - some of the concerns around resistance may be overplayed.
Ben Weil
I do think to some extent antimicrobial resistance has been overstated as an issue in relation to DoxyPEP or perhaps what I would say is it is routinely trotted out as the foremost argument against DoxyPEP, sometimes by people who have other complaints about the use of DoxyPEP.
What I mean is that what we know already about DoxyPEP and antimicrobial resistance isn't worrying.
Phil Samba (Host)
And there you have it, antimicrobial resistance is a concern, but it isn’t an issue yet.
This was reminiscent of when PrEP was first making the rounds. There were concerns about STIs going up, and funnily enough, antimicrobial resistance going up as a result of that, and those things didn't happen.
Ben Weil
So for instance, we've seen very, very similar responses and reactions in the early days of HIV PrEP when HIV PrEP was floated out, people had lots of, you know, in part reasonable concerns about upticks in STI transmission because of what they feared were declines in condom rates. But alongside that, we also saw really speculative anxieties about things like HIV superinfection or resistant strains of HIV, none of which have borne out into reality.
And those conversations weren't had in sort of rational, reasonable, moderated ways. They were had in ways that were established to gatekeep PrEP from the communities that might benefit from it. And similarly, what we're seeing here is conversations about antimicrobial resistance being used to deny, slow the rollout of, or gatekeep DoxyPEP from communities that might benefit from it without positing or forwarding solutions about how we might actually and practically monitor and sensibly control the rates of antimicrobial resistance.
Phil Samba (Host)
Careful monitoring can make sure antimicrobial resistance doesn’t become an issue. Interestingly, Ben also saw those similarities between the early days of PrEP and where we are now with DoxyPEP.
Ben Weil
So I've already mentioned that there are some quite striking similarities in the, let's say, discursive landscape of DoxyPEP and HIV PrEP. For instance, we can see anxieties about unlimited condomless gay sex being expressed in the case of DoxyPEP through anxiety about antimicrobial resistance and similarly in the context of HIV PrEP those anxieties were expressed through anxieties about HIV superinfection or STI transmission.
Phil Samba (Host)
The fear around STIs was unjust.
STI rates have gone up but according to data from UK Health Security Agency, so have the number of sexual health screenings. In fact, HIV testing was the highest it has ever been in 2022.
More testing will contribute to more STIs being found, and the sooner they're found, the sooner they can be treated.
So yes they’ve risen, but mostly because more people are getting tested.
In the very same report, UK Health Security Agency also said that comparisons of STI trends over several decades should be made with caution given increases in the population size and in testing for STIs using more sensitive diagnostic tests over time.
Phil Samba (Host)
So amid all of this people have little choice but to buy DoxyPEP online. Does this also sound familiar?
Queer people finding a way to get medically safe drugs, that protect them and their sexual health - even though it’s not prescribed on the NHS. A community taking action to get it into the hands of those who need it most?
Yeah, it sounds familiar to us too.
For over 40 years there’s been a strong focus on being at risk of STIs in the community however, DoxyPEP might be the thing that changes that forever.
We’ll tell you more about it after the break.
Phil Samba (Host)
With all these new advancements in sexual health such as DoxyPEP, it makes me wonder why things aren’t different this time around.
Everything we’ve covered over the last few episodes is a clear call to action on the lessons we should have learned from the fight for PrEP. But what have we learned?
Let’s ask Will Nutland from The Love Tank.
Will Nutland
And if there's anything we've learned from HIV PrEP, it's that if we don't implement these new technologies in an equitable way and in a quick and a swift way, then those of us that have both the economic and a social capital to go and find them ourselves will do so.
And that means we might not be using those prevention methods in the most, in the best possible, the most safest, the most effective way. But it also means that those people who have least social and economic capital will be left out of the benefits of these new technologies.
And as I've been saying for pretty much the last decade, we will have collectively failed if all we do when we see these new technologies is the technologies, the medicines, the vaccines only going into people like me, older cis, gay white men living in places like London.
Phil Samba (Host)
So there you have it. The change we want to see happen is very doable but a choice needs to be made. We again have the tools to better our sexual health but we’re not using them, we’re seeing this happen again with DoxyPEP.
What are the potentials for ending HIV and solving other future sexual health issues before they become just like the ones we’ve had in the past?
Will Nutland
So the last two years with MPOX and Monkeypox, as it used to be called, has demonstrated once again not only the resilience of our communities but how we've been challenged once again with another health outbreak.
MPOX showed us how government intransigence, how ignorance through stigma, through discrimination, once again impacted on our communities. The media tried to demonise people.
The media tried to demonise people, the media tried to portray MPOX as being something that disproportionately impacted on people who were having lots of sex or involved in sex work, or people who were foreign, or people who were being carefree.
And these were all the kinds of things that we saw with HIV. But as communities, we were ready, we were ready to respond and ready to respond in a number of ways.
Phil Samba (Host)
The resilience of queer people repeatedly comes up whenever talking about our health but most of the time that resilience comes from us not being heard. That’s why, for Will, it's vital to listen to people from marginalised communities who are often left out of conversations.
Phil Samba (Host)
Organisations like The Love Tank were quite literally at the forefront of those discussions and conversations with government, with statutory decision makers, with people in our National Health Service, to ensure that our voices were heard, that we were listened to.
And also more crucially to understand that when we heard inaction from those institutions, because of our experiences in the history of HIV, when we heard that inaction, we expected that inaction to mean that people didn't care for us or weren't doing anything about this health crisis.
It turned out that wasn't the case and it was a brilliant historical learning moment for lots of those people in those institutions that silence quite literally for many of us equals death.
And we've been able to do work with lots of those institutions to reinforce the importance of communication too and with communities. If you don't tell us what you're planning to do, we will assume that you are planning to do nothing.
And so once again, just like with the crisis response to HIV, community organisations stepped up. We produced educational material. We went and met with places like sex venues and made the case why those sorts of venues should not be closed down, but instead were crucial and important assets and allies in what we were trying to do in the response to MPOX.
Phil Samba (Host)
We’ve talked about the how we finally made PrEP available and have since had two more sexual health issues dealt with incorrectly. Why hasn’t the NHS learned its lesson?
Deborah Gold
I think fundamentally the starting point is sexual health services, well-being services are chronically underfunded.
Phil Samba (Host)
Deborah Gold, outgoing CEO of National AIDS Trust.
Deborah Gold
And that seems like an easy thing to say, but you can't really make any progress until you deal with that problem. Everything comes back to that in the end. And then, you know, if the funding and then the second thing I think is the way that HIV and sexual health services and maybe kind of wider services are seen.
And so I think there's the second piece of the puzzle is like a fundamental shift in how we view public health and prevention and how we prioritise it so that it's seen as having parity of esteem, next to treatment in NHS services.
I think this really boring kind of technical thing about splitting off the way that these services are funded, delivered and commissioned actually leads to real kind of disintegration of the way the health service works, the way people are able to integrate and take advantage of innovation, the way, you know, and I think lots of the problems that exist and the opportunities fundamentally won't get solved until those two things happen.
Phil Samba (Host)
We talked about it in the last episode but I think it is important to discuss institutional racism again - because that bigger picture affects health for people of colour in all settings.
Deborah Gold
I mean, racism is bigger than health services. And so there's kind of bigger question about dismantling systemic racism where I think there's kind of limits to what a health system can do inside a wider system that systemic racism exists in. But first of all, I think it can understand the reasons for migration, welcome them and expand what I think is really one of the really positive things about HIV and sexual health services, which is anyone from anywhere can access them more widely in the health service to enable access to be clear.
I understand racism and migration are not the same thing. So that's one thing. And then I think the other thing is taking what's kind of worked, I think, well in terms of HIV, which is allowing what needs to happen to be led by people affected by HIV and doing the same thing in terms of racism.
It has to be led by people that experience that racism that can talk about what a service needs to look like in order to meet their needs. And that's the case generally, you know, kind of the more you provide generic services that are targeted at everyone, the more those services will only ever meet the needs of the people who have the least need because it goes into the medium.
And so, if you want to dismantle systemic racism, you have to look at the system, you have to ask the people who are affected, you have to listen to them, tell them about what you need. And then you have to have a service that is staffed and funded to enable it to flex in that way.
I appreciate that answer is quite broad and it doesn't kind of focus on specific things. I think, you know, there are individual things that we could start doing now, even without those kind of big-level changes.
And, but that involves taking individual things. This, you know, this whole podcast series has been about PrEP and access to PrEP and, you know, kind of looking specifically at access to PrEP. We know that you know, kind of black African women are at particular risk of acquiring HIV, but they're not accessing PrEP.
Phil Samba (Host)
Often in the HIV and sexual health sector, you hear the phrase “hard to reach communities” - but it’s not only a misnomer, the phrase is damaging the mentality about our approach.
Most health professionals don’t like to admit it but reflecting diverse audiences can be challenging for them.
It’s difficult especially if they don’t come from those communities or understand how to reach us effectively.
I’m sick and tired of being told we are hard to engage and hard to reach, there are NO hard-to-reach communities, there are ONLY hard-to-reach services.
Deborah Gold
And so we need to think about making it available in places where they may go. We need to think about empowering other types of clinicians to be able to have conversations about PrEP and about HIV. So for example, in the new women's health hubs or in abortion services or when somebody is going to have their diabetes checkup.
And, you know, that means taking away this kind of mysterious stigma that exists around HIV in health services themselves, it's not good enough anymore for clinicians to feel afraid of talking about HIV to people. It's not good enough for them to use as an excuse that they don't know about HIV, they're not experts, leave it to the experts, because that always means it's something that happens to other people over there.
And it builds into that idea. So I think there's action we can take now, an online service that allows people to maintain that anonymity services in a way that's convenient to them where they don't have to physically go to an inconvenient place at an inconvenient time and wait in a queue for hours. So you know there are practical things we can do and then there are bigger things we can do around the system that are longer term.
Phil Samba (Host)
This can, of course, all be applied to trans and non-binary people’s health too.
Deborah Gold
Largely speaking, healthcare for trans and non-binary people is so poor that it's really actually frighteningly easy to see how it could be improved. And it starts by like a basic, you know, basic human decency and respect of like treating people as the people they are and starting from that point.
The current environment, the media environment, the politicisation of trans identities and bodies and needs means that it's a really difficult time to be a trans person. It's a horrifyingly difficult time to be a young trans person. And all of that can't help but affect healthcare.
And then even some of the good things that have been built up over time are starting to be dismantled without new things necessarily being put in place. But I think, you know, if you step away from the politicisation of it, we do have models of effective trans healthcare that are holistic, that we have seen have worked.
And it's not rocket science. It's the same as works for all kinds of different communities who are, you know, poorly affected and able to access things. And it's about giving the space and the openness as well as the funding to allow self-organisation.
Phil Samba (Host)
Spending what time I have in the sexual health sector too, shows me the power in sexual health and specifically targeted services run by and for the communities themselves - it’s something we lead with at The Love Tank and time and time again delivers results.
Deborah Gold
So, you know, kind of services run by trans people, for trans people, in places where they feel comfortable going, understanding that. I mean, we're talking about trans people now, but this is often true for everybody. You know, individuals often don't experience healthcare problems in neat little buckets.
You know, this thing's about my HIV, this thing's about my sexual health, this thing's about my mental health, you know, or my kind of my concerns about how I'm using alcohol or drugs. So putting those things together, making sure that people feel confident and comfortable that they won't have to explain their bodies, justify their gender, be misgendered, be dead named before they even kind of get through the door.
I think is the answer to that. And then providing those HIV and sexual health services within that environment. And we know that that works because it's happening now. We just need more of it.
Phil Samba (Host)
In 2019, the government committed to an ambition of ending new HIV transmissions, AIDS diagnoses and HIV-related deaths within England by 2030 but this is lip service without enough funding or dedicated people in the government who care about improving the sexual health of marginalised communities.
Florence Eshalomi MP
Hi, I'm Florence Esholomi. I'm the Member of Parliament representing Vauxhall in South London. Vauxhall covers Brixton, Stockwell, Kennington, Oval, Waterloo. I got elected at the last general election in 2019 and I'm also one of the co-chairs of the All Party Parliamentary Group on HIV and AIDS.
Phil Samba (Host)
That's Florence Eshalomi who was elected to the constituency in 2019, she's been an incredible ally to us.
Florence Eshalomi MP
One of the things that drew me to join in the APPG was the fact that it's one of the longest, I think it is the longest-established all party parliamentary groups. It was set up in 1986 or 87, I think it was one of the first APPGs. And it was, you know, it was set up during the height of the AIDS campaign and the AIDS virus in the 80s.
So you saw parliamentarians from all different political parties, from both the House of Commons and the House of Lords coming together across the political divide looking at how they can fight for the rights of people living with HIV and AIDS. And the reason I wanted to get more involved in the All Party Parliamentary Group, I think for a long time it's been perceived that HIV and AIDS is a white LGBT male issue. It's not.
Phil Samba (Host)
It makes my heart smile knowing there are people in the government who really care and truly understand the situation we’re in. The fight is not over.
Florence Eshalomi MP
And it's always also being perceived that HIV, you know, we've addressed it, we've solved it, you know, it's fine, it's not.
And when I saw some of the statistics and it was showing that some of the groups that continue to be affected in, you know, in modern times are black women, looking at the fact that the experiences of black LGBT men living with HIV and AIDS, I said, you know, this is something that I really want to get involved in and look at how I can use my role as a black female MP to advocate some of the issues that they're grappling with and making sure that their voices are central to us fighting HIV and AIDS and making sure that the UK is one of the first countries to end new transmissions by 2030.
Phil Samba (Host)
I was curious to hear what Florence thought about the government’s responsibility in addressing the current HIV epidemic. Is this something they should do something about?
Florence Eshalomi MP
We have to look at how Parliament leads the way in terms of policy, in terms of investment, in terms of medical treatment, in terms of investment for support for people living with HIV and AIDS, in terms of investment for organisations without those organisations on the ground, you know, supporting fantastic people parliament has to lead the way in ending some of the stigma that still surrounds HIV and AIDS. So I think as the lawmakers, Parliament has a key role in all those areas.
And also to increase dialogue between people living with HIV and AIDS, not just in the UK, but around the world. This is a global issue. And as the UK Parliament, as part of the international community, and one of the founding members of the Global Fund, we've got a key role to play in that.
Phil Samba (Host)
So - what would Florence like to see next in sexual health provision?
Florence Eshalomi MP
One of the things I'd really like to see when it comes to sexual health, first of all, is around adequate funding to support sexual health clinics right across the country. Depending on which part of the country that you live in, some places there are absolutely no services available and it's really important that people are able to get access to good confidential advice in terms of their sexual health.
I think we also need to look at education in school around teaching young people around HIV as well and why it's important to have safe sex and really being honest about that and talking about some of the things around that.
So it's not just about yes, use a condom. It's about all the things and why it's moved on from that. In terms of the campaign and fight against HIV, it's about how we work to ensure that the UK is on course with the HIV action plan that was adopted many years ago to continue to work towards that goal of ending new HIV transmissions.
And that will only happen if we have campaigns around getting tested. We know that in February it's HIV testing week. That will only happen if we have campaigns around ending the stigma of HIV and AIDS. That will only happen if we have adequate support for some of the disproportionate communities that suffer.
So LGBT and trans women, LGBT men and trans women, BME women, black women. It's really important that their voices are central and involved in some of these things. And last, it's important because we have to remember that the UK has a role to play, not just in what happens here but internationally as well. So what I'd like to see is the UK continue to make sure that this is a key agenda for us.
Phil Samba (Host)
And there you have it, the historic battle that many people still don’t know. Yes, we have PrEP available but still, so much work needs to be done.
What I found interesting about making this podcast series was seeing how much we haven’t learned from our past. Fighting for access to PrEP was reminiscent of fighting for access to HIV medication in the 90s.
Fighting for PrEP for nearly five years before it was made available on the NHS
- is reminiscent of many other queer and broader sexual health fights happening now, from access to gender-affirming care to DoxyPEP.
Across this series we’ve discussed the history of HIV medication and the start of PrEP, bareback porn in the 2000s, the generational divide with PrEP, the Proud study, the origins of PrEPster and IWantPrEPnow, queer community activism, the Impact trial, National AIDS Trust winning the court case, Truvada whores, condomless sex, how HIV services have changed, why PrEP hasn’t made as big of an impact on HIV in the global south, National AIDS Trust going back to court, institutional racism, trans healthcare, PrEP access issues across intersectionalities from black communities to white gay men.
And after that whistle-stop tour of the HIV sector and the fight for PrEP - yes we do have PrEP on the NHS but what’s clear? We still have more to do. It’s very much not over.
As a community, as a society - and in the halls of power - we need to listen better. To people who work in the field - but more broadly - people who need the help. They are best placed to guide us on how service and provision can help change lives and revolutionise sex. They know this, because they live it.
That’s the only way we can actually make the changes that improve queer health. That improves sexual health - for everyone.
PrEP has been available in England on the NHS since March 2020 - and in over four years there are still so many people and groups who need access to it, who can’t for a number of barriers, reasons and nuances depending on their age, location, sex, identity, or background.
Meanwhile - this whole documentary sits on a bigger issue of the need to eradicate HIV stigma which is still very prevalent.
Indeed, just creating a sense of calm that everyone who is having sex should be testing for STIs regularly - from GP visits to sexual health clinics. People shouldn’t feel embarrassed or uncomfortable to get tested.
That’s part of a wider issue of sex shaming, tied to internalised shame, LGBTQIA+ phobias and prejudice - and just society’s broader - eeep, around talking about sex.
And don’t get me wrong - The Other Blue Pill has played a huge part in changing our lives, for all of us.
It’s lifted and liberated so many of us from the fear of HIV.
It’s saved so many lives that could have otherwise been lost or changed forever by HIV.
And now? It’s time for the next healthcare innovation to take us a step further.
That’s something I know won’t be far around the corner either, with tireless activists, community groups, sexual health organisations, scientists and people like you - who listened to a series to better understand our history, to learn from the lessons from our past.
And yeah - anyone who pops a pill every day to look after themselves and the health of those around them - people like you who care and love your community.
That’s the legacy of The Other Blue Pill - it’s a movement of everyone in the PrEP generation who said:
“I’m prepared to take steps to protect me and my partners - are you?”
I’m Phil Samba, and this has been The Other Blue Pill.
The Other Blue Pill has been a QueerAF production for The Love Tank, hosted and researched by me, Phil Samba, with additional scripting, plus production from Jamie Wareham. The show has been supported by the National AIDS Trust.
For more resources about PrEP, show notes - and to read more about queer health and understand the LGBTQIA+ world, visit wearequeeraf.com/theotherbluepill