TLDR: While the Levy Review correctly identifies some of the issues with Gender Dysphoria Clinics, its recommendations tinker around the edges – rather than solving them. Reporting by Vic Parsons, and Jamie Wareham.
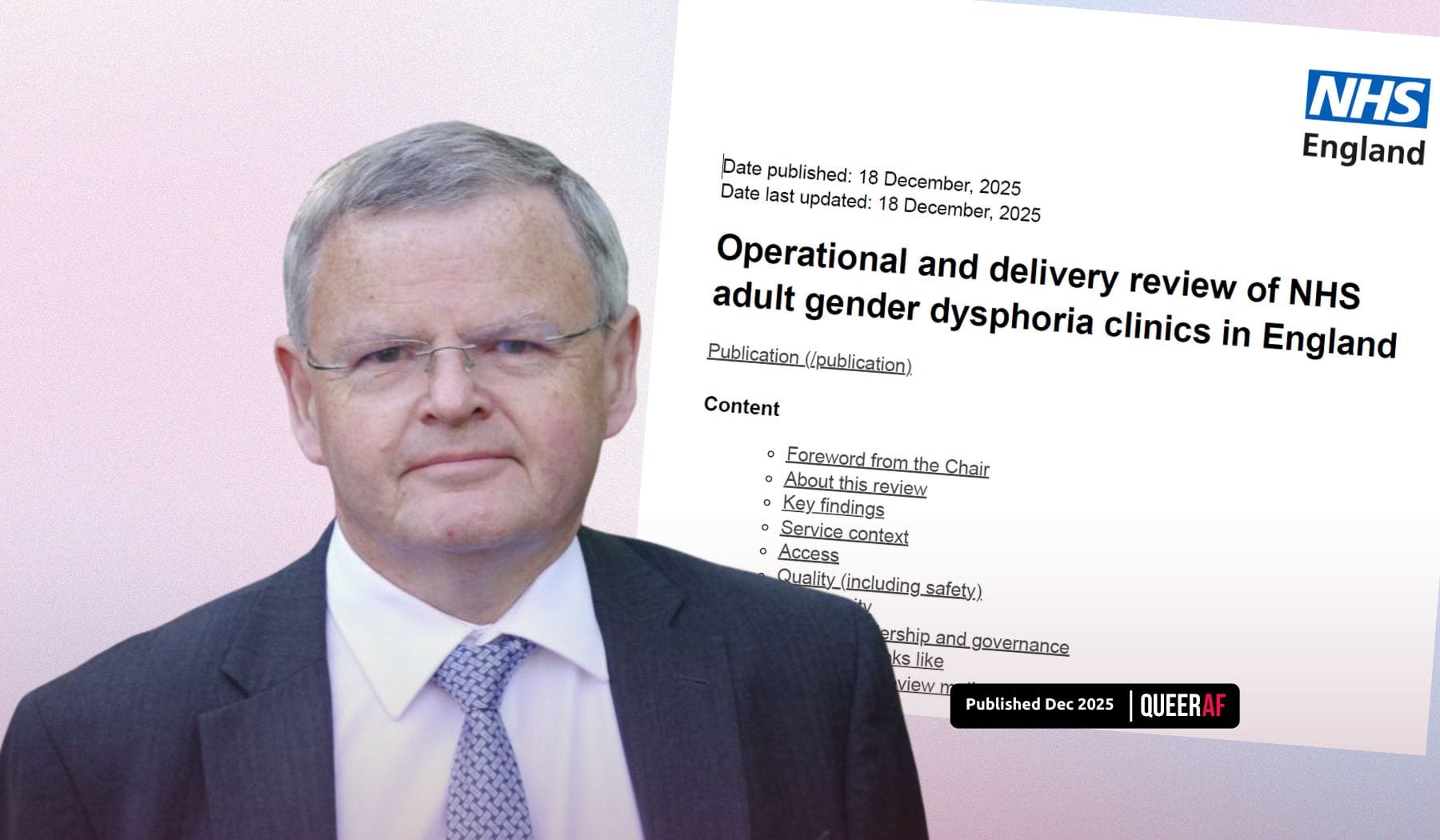
Most NHS gender clinics have “exceptionally long waiting times” and all require “immediate improvement” to be fit for purpose, according to a review of adult Trans+ healthcare services in England carried out by Dr David Levy.
In a 65-page report, Dr Levy identifies dozens of issues with adult gender clinics, from less than a third of discharged patients having completed their treatment to a lack of data on patient outcomes and insufficient training for healthcare workers in the wider NHS around caring for Trans+ patients.
In 20 recommendations for improving adult gender services and addressing bottlenecks in the system to reduce waiting times, Levy urges gender clinics to work with GPs and local health boards to improve consistency and access to Trans+ Healthcare.
What are the Levy report's key recommendations?
Its key recommendations include creating a national waiting list for adult gender clinics, ending the practice of self-referral, discharging patients waiting for surgeries back to their GP, raising the referral age for adult clinics from 17 to 18, and creating a national gender board that will oversee Trans+ healthcare – which would be chaired by Dr Levy.
The review acknowledges that “hearing directly from transgender patients significantly enhanced our understanding of the services”. However, it does not go as far as suggesting abolishing gender clinics and moving to a system of informed consent in primary care – the solution long advocated for by Trans+ experts as the most realistic.
The recommendations will also retain the requirement of a diagnosis of gender dysphoria, despite it being removed from the International Classification of Diseases by the World Health Organisation in 2019.
“Faced with the sinking Titanic of trans healthcare in England, the Levy Review suggests we rearrange the deckchairs,” Dr Ruth Pearce, a transgender health expert and Senior Lecturer in Community Development at the University of Glasgow, tells QueerAF. “Levy's report offers a limited, technocratic response to the ongoing crisis, recommending a range of bureaucratic measures to improve the efficiency of the current system.”
Trans+ researcher Dr Cal Horton, of Oxford Brookes University, concurs: “[The review] fundamentally fails to deliver meaningful improvements to trans healthcare”.
“At its heart, it maintains and reinforces a system built on clinical control of and power over trans communities,” Dr Horton said. “There is no effort to improve accountability. No recognition of institutional transphobia. No recognition of clinical violence.”
The review urges the NHS to change the way patients receive hormone replacement therapy (HRT), suggesting that hormones should be prescribed and monitored by a gender clinic for the first year of treatment for more consistent care and monitoring while hormone levels stabilise.
After this first year, patients would be cared for by regional hormone teams in primary care hubs where specialised GPs, known as “GPs with extended responsibility”, or GPwERs, take on responsibility for blood level monitoring and prescribing. There is no mention in the report of what this will mean for Trans+ patients who currently access hormones through bridging prescriptions, shared care with private clinics, or who self-medicate through DIY avenues.
The report suggests that senior clinicians travelling to provide treatment to Trans+ people in prison or other institutions – who are already routinely denied access to HRT – is “not a good use of limited clinical resources”, raising concerns that the already limited Trans+ healthcare provision for those people will end.
It also suggests that first appointments at gender clinics should be carried out by senior clinicians, rather than non-medical staff, as is often currently the case – which could have the opposite effect to reducing waiting times.
Echoing research and investigations in the ‘Gender Clinic Files’ published earlier this year by QueerAF in collaboration with What The Trans?! and Claire Prosho, the Levy review suggests that new gender clinics must be geographically spread out to ensure more even access, noting that some patients travel long distances for appointments.
The review also notes the lack of data in many areas of Trans+ healthcare – a gap that Prosho sought to fill by making the Freedom of Information requests that resulted in our investigative series.
Speaking to the Press Association ahead of the review’s release, Levy said he’d “walked through the minefield” producing this report, and thanked the clinics for their co-operation. “This is about getting things better for the patients, getting things better for the staff,” he added.
What’s the response been to the Levy report?
NHS England welcomed the review, as did the Health Secretary, Wes Streeting. In the NHS’s letter to Levy, it set out how it committed to the vast majority of recommendations, including raising the referral threshold, ending the limited self-referrals, creating new GPs with Extended Role in Gender Medicine (GPwERs) and changing the surgical pathway so that patients can be discharged earlier.
Streeting, in a parliamentary statement, also committed to the National Waiting List measure and lambasted the “poor productivity” in the system. He additionally acknowledges that it signals “the urgent need for an expanded number of services.”
The LGBTQIA+ sector had a more mixed response; for most, the report fails to address the issue and simply “tinkers” around the edge of a system that does not serve the patients it supposedly provides healthcare for.
Tammy Hymas, Policy Lead at trans rights organisation TransActual, said: “We are concerned that this review is a missed opportunity to give all trans people timely and local access to gender affirming hormones on the basis of informed consent – the most effective way to clear eight-year-long waiting lists.”
They set out how, given the acknowledgement from Streeting that Trans+ people are being failed by the NHS, the review should prompt the government to “turn words into action and provide long-term funding to end this crisis.”
Gender critical organisations expressed anger that the review didn’t recommend major restrictions on Trans+ healthcare, like the Cass Review before it. Many Trans+ people were afraid of that outcome ahead of the Levy Review’s publication; instead, it highlighted the value of talking to Trans+ people to inform its conclusions about this community's needs.
Analysis: Now we wait and see what this all actually looks like
What could this all mean? The proof will be in the pudding.
Part of the reason the Cass Review was so devastating was it had generated a captive audience of gender criticals and NHS staff with a willingness to decimate Trans+ healthcare for young people ahead of its publishing. This was clear from how quickly NHS England changed specifications, the government banned puberty blockers and parents began facing safeguarding referrals.
This review, which dropped hours before the parliamentary recess for the Christmas holiday began, recommends what many see as sensible but limited actions. It’s a long way from having the kind of immediate impact of the Cass Review.
Still, there are questions to be answered. How will more training from an undergrad level up in providing healthcare to Trans+ people impact the whole NHS system, not just gender clinics?
And indeed, as the government continues to blindly pursue ‘AI improvements’ amid rising unemployment, using LLMs with biased training, what will this report’s recommendations to use AI to transcribe interviews and handle admin mean? With Levy raising lack of data on patient outcomes as a concern, trust must be rebuilt with Trans+ patients to begin collecting data in this way.
So, the takeaway: this is not a decimation of care as many feared it could be. It mostly recommends harmless, possibly useful ‘tinkering’, but ultimately it advocates for change to a system set up by cisgender people which fails transgender people and their health.
As Dr Ruth Pearce told QueerAF, “Levy fails to tackle the most fundamental problems with the gender clinic system: gatekeeping, pathologisation, and dehumanisation, which all harm patients while also wasting clinical time and resources.”
The changes it recommends are not radical enough to give Trans+ people the care they deserve and desperately need.

We worked with a team of 15 Trans+ researchers, journalists, advocates and our partners at What The Trans!? - to rapidly unpack the ramifications of this critical report.
That means what you're reading this week is not just reporting by Vic Parsons and me - it’s a collective community effort to help you understand the Levy Report.
That's how we approach everything we do at QueerAF. We build movements, coalitions and connections - so we can unify forces against the rich and powerful anti-rights forces.
Before we launched, we conducted a comprehensive consultation with community leaders and media professionals. When we created our What The Pox? documentary, we listened far and wide about how we could best show up - an approach applauded by the WHO. In supporting Trans+ History Week as one of our launchpad projects, we met with 20 LGBTQIA+ sector organisations and to get their buy-in and support to ensure the organisation had a strong foundation to begin.
That's what media should look like: embedded in and playing a crucial role within the community we set out to serve.
No other gay media works like we do. That's why we need your support. If you believe our model is how you'd like to see all of the media run - vote with your feet, and your cheque book.
QueerAF members make our unique model possible. Please, upgrade today.